
What our report means for people who use services, their relatives and carers
In Right here, right now we looked at crisis care services in England, focusing on what it is like for people having a mental health crisis.
Accessing the right help, at the right time
We reviewed people’s experiences of help, care and support from GPs, specialist mental health services and accident and emergency, as well as when they are detained under the Mental Health Act.
Regardless of which service they came into contact with, most people told us that the care they received did not help to resolve their crisis or was only partly helpful.
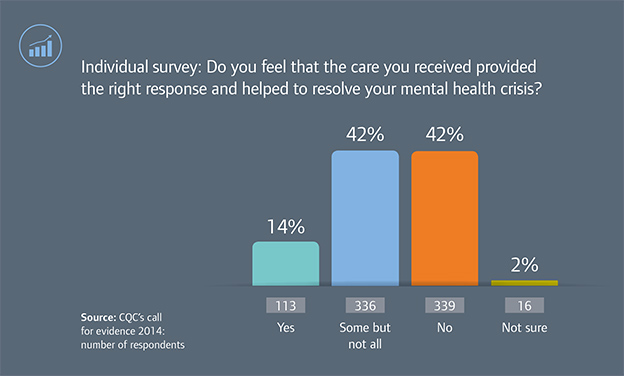
We think this is unacceptable. Services need to make sure they have the expertise to support people in crisis, listen to the needs of each person, and provide appropriate support for that person quickly.
GPs are the main point of contact for many people in crisis. On the whole they gave people the help they needed, when they needed it. Voluntary services were also seen as being accessible at a time of need, with 74% of people in our call for evidence saying they received the help they needed quickly.
However, more than one in four people said that they did not get the help they needed from their GP.
“I feel that GPs dismissed my concerns and my experiences and made me feel that I could not turn to them.”
Not being able to access the right help at the right time is not acceptable. It could mean that people have to use services, such as A&E, that are not the best placed to meet their needs.
People also told us that trying to get help in the evenings and at weekends was a big problem. Many did not know where they could go in their community, or had to wait a long time in A&E before being seen by a mental health professional. Again, we think that this is not fair or acceptable – someone with a broken leg would not expect to have to wait to be seen. It should be the same for people in crisis.
Crisis services should be caring
How people were treated when they went for help had a huge impact on their experience. We found that the quality of care people receive varies depending on where in the country they live and which services they come into contact with. It is not good enough that where a person lives has such an impact on the care they receive when they are in crisis.
In general, people told us that they felt respected by services. Again, voluntary services scored highest, with 87% of people in our call for evidence saying that they felt respected, and that they were least likely to feel judged. GPs also scored well in these areas, but A&E was the place that people said they were most likely to feel judged.
“I have a clinical illness. It’s not my fault my brain chemistry fluctuated… To be treated as a drunk, an inconvenience and with visible contempt only makes it worse.”
Many people who went to A&E because they had self-harmed had had a negative experience, although some people gave us positive examples as well, with one person telling us:
“When booking in at the A&E reception, I was allowed to write down my self-harm injuries rather than give the information verbally, which could be overheard by other people.”
People’s experiences of community mental health teams and crisis resolution home treatment teams were also mixed. Our call for evidence showed that there seemed to be a 50:50 chance of people getting the care they have a right to expect, and that their experiences often depended on who saw them.
Some of the most positive stories we heard related to the police. It is encouraging that a non-healthcare professional can get it right. This should act as a challenge to those working in the health service to do the same.
“[I had] brilliant support from the police who gave me good advice and agencies to contact.”
People and their carers should be involved
“I felt like an object, not a person. I was passed from person to person, organisation to organisation. Spoken about, not to.”
Everyone who uses mental health services should be considered as partners in the care planning process. They should be actively involved in making decisions about their care. However, almost a quarter of the people who responded to the 2014 Community Mental Health Survey said that they had not agreed the care they would receive. A substantial minority told us that they did not feel involved enough in their care planning. This is not good enough and raises serious questions about the quality of care these services are providing.
Carers also told us in our call for evidence that they feel excluded and not listened to by health professionals.
“It’s very hard to say, as a carer, what I felt about the service provided during my son’s most recent crisis as I was almost totally excluded from it.”
Carers are a vital, and unsung, part of the health and care system. They often have knowledge about the person, their home and the ways that person’s crisis could be managed. They should be involved in this process.
What we are calling for
We recognise that people’s experiences of crisis care are unique and extremely personal. Services have a key role in shaping their experience and need to make sure that they do what they can to help a person through this very distressing time.
The recommendations in our report are aimed at the people responsible for commissioning local services. They must make sure that there is a coordinated and system-wide approach to improving the experiences of those in crisis. Commissioners need to look at the make-up of their local populations and commission services to meet their needs.
We also encourage:
- Community mental health teams to make sure that they involve people in decisions about their care, and support people to develop a crisis care plan.
- Specialist mental health services to make sure that crisis helplines are available when they are needed and provide people with the right support.
- Commissioners to make sure that crisis resolution home treatment teams are resourced properly and can respond to people at any time through home treatment visits.
- Acute hospital trusts to make sure that A&E departments are warm, compassionate and empathetic to people who have self-harmed.