Acute hospitals
To review infection prevention and control (IPC) in acute hospitals, we analysed the outcomes of the Emergency Support Framework calls between our inspectors and all acute and specialist trusts. These calls discussed each trust’s ‘Board Assurance Framework’ to identify how the trust was assuring itself of good IPC across 11 key areas.
Broadly they said they had high assurance across all the areas (see figure 1).
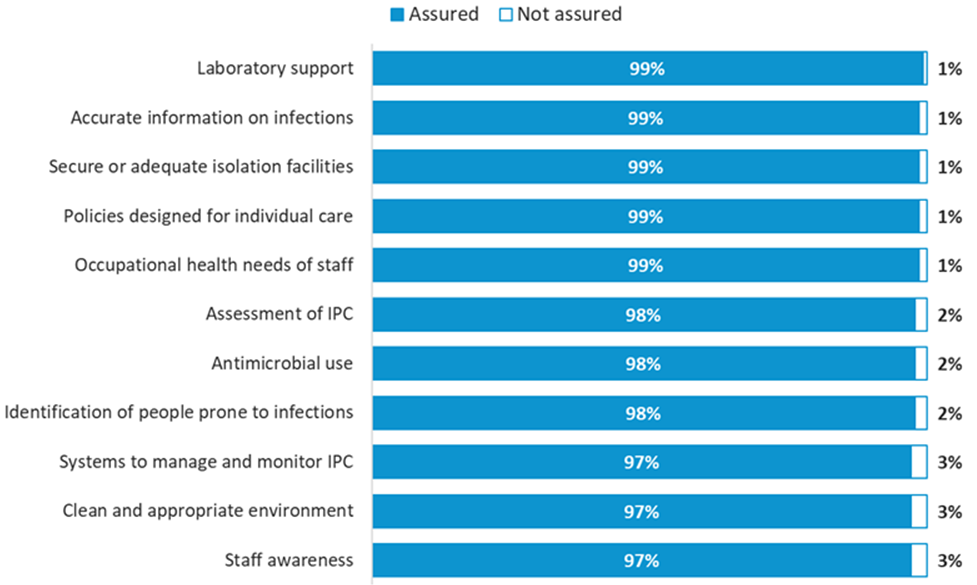
Source: Emergency Support Framework responses from 138 NHS acute trusts across all questions. Responses from the remaining four trusts were incomplete at the time of reporting (15 September).
Gaps in trust assurance
While most trusts assured themselves that they were managing IPC systems and mitigating risks, there were some examples of where the systems and procedures were ineffective.
There were a few trusts with ineffective systems to manage and monitor IPC. Robust audits were not always taking place during the peak of the pandemic, including audits of personal protective equipment (PPE), waste disposal and the screening of other healthcare-associated infections. Where audits were taking place, there were a few examples of trusts not being able to show any learning from them.
Oversight of IPC training varied between trusts, meaning some trusts could not always be assured that staff had been adequately trained in IPC procedures. Non-clinical and non-ward staff were not always provided with COVID-19-specific training or guidance. In one example, the trust was unaware of the IPC training or guidance that contractors had received or whether any had been provided at all.
Some trusts had challenges that limited their ability to isolate and cohort COVID-19-positive patients. Insufficient side room capacity was commonly reported, particularly for trusts with older estates, as was limited ventilation. Trusts that were able to provide assurance, despite an older estate, had carried out robust risk assessments and put mitigation plans in place, for example using pop-up isolation facilities, repurposing other areas of the hospital for COVID-19 patients and adding doors to the entrance of bays.
Good practice and innovation
Trusts reporting that good systems were in place to respond well to the pandemic said that they implemented gold, silver and bronze commands to provide good governance and oversight. While some trusts suspended audits during the pandemic, others maintained these throughout, especially around antimicrobial stewardship, cleaning and hand hygiene. This enabled board assurance.
Trusts had implemented front door triage and streaming systems to categorise patients, often into RAG-rated systems (red, amber, green) to ensure their safe movement throughout the hospital, alongside new swabbing protocols. Relevant polices had been reviewed, updated and were well communicated among staff, patients and communities. Most cleaning regimes had been reviewed, with increased targeting in high-risk areas.
Where trusts told us about their good practice and innovation during the pandemic, certain topics stood out.
IPC teams
Where trusts had established well-staffed IPC teams, these held a vital role intrinsic to delivering good IPC. IPC nurses and chief nurses were available at all times. Some trusts had put extra resource in place (creating seconded posts) and included experts such as microbiologists and virologists. One trust had recruited an additional 24 IPC safety officers, which included previous cabin crew because of their expertise in safety and customer care.
IPC teams led in a range of key areas:
- risk assessments
- identifying and communicating changes in guidance
- identifying issues on wards and putting mitigations in place
- carrying out audits
- acting as the link between ward and board
- helping to ensure compliance by being visible on wards and advising around PPE, fit testing and hand hygiene
- training cleaning staff, including cleaning contractors.
If areas of learning are identified, the IPC team will immediately attend to the ward and organise education for the staff.
PPE
PPE was a challenging area throughout the height of the pandemic. Issues included the pace of change of PPE guidance and the challenge of there being multiple suppliers of PPE – for example, different types of mask needing separate fit testing. However, there were strong examples of partnership working in response. Trusts supported each other with supplies and some of them worked with the fire service to help with fit testing. ‘PPE safety officers’, ‘COVID champions’ and ‘donning and doffing buddies and videos’ were used to keep people up-to-date and ensure compliance.
Where we were told of good practice, trusts had got to grips with the pace of change in PPE guidance and ensured this was understood and well communicated throughout the trust.
The trust deployed a roving team to deliver in-situ training on PPE. When national shortages of PPE impacted supply, it implemented a roving fit testing team.
Some trusts came up with creative solutions to PPE challenges, for example working with volunteers to produce more than 27,000 gowns, and manufacturing their own visors, hand gel and dialysis fluid when there had been a national shortage.
Wellbeing of staff
Wellbeing initiatives for staff have included providing quiet spaces, called ‘wobble rooms’, for staff to take time out.
There were examples of having tissue viability nurses and dermatology support on hand for staff suffering skin damage due to the use of PPE. One trust had a psychologist based in critical care that staff members could access, as well as a psychologist doing daily ward rounds. Trusts told us that they provided hotel accommodation for staff so they could continue to work while allowing people to shield in their households.
Efforts have been made to keep in touch with shielding staff and those on maternity leave so they still felt part of teams and were kept up-to-date.
The trust was running ‘keeping in touch days’ in local parks for staff on maternity leave, which included their families, to keep up-to-date in a safe environment.
Most trusts had put in place daily communication bulletins for staff or had improved existing communication methods.
Supporting patients and visitors
Visiting has been hugely restricted throughout the pandemic, so trusts have set up a range of systems for people to keep in touch with their loved ones, while preventing infection. This included using tablet computers on every ward, and providing drop-off services so families could leave patients the things they may need. One trust increased the number of volunteers they had to help patients with online communication, while another identified patients who did not have any relatives and nominated a member of staff to write them letters. Another employed staff to sit with dying patients to make sure no one died alone.
As restrictions have been lifted and some visiting resumed, this has taken place in outside spaces or by appointment. Visitors are given information on websites and through clear signage, and meet and greet services ensure masks are worn and social distancing is maintained. For example, one trust employs ‘pandemic receptionists’ to ask screening questions and provide PPE.
Meeting demand
Trusts reported high levels of activity to redeploy staff and repurpose spaces to meet the changing demands on the service. Staff were moved to work in high demand areas, such as critical care, or worked to support testing and tracing and PPE supply.
Wards were changed to provide additional intensive therapy unit beds or to support cohorting and social distancing measures. In one example the trust converted their sexual health clinics into testing facilities. Another worked in partnership to use the local football stadium to house antenatal clinics, pregnancy scanning and a maternal day unit, so that these services could be provided outside of the hospital environment.
System collaboration
The pandemic represented a shared goal and saw trusts unite with local systems to ensure a coordinated response, which they committed to maintain beyond the emergency. There were positive examples of routine collaboration between neighbouring trusts, local authorities, clinical commissioning groups, primary care and care homes to ensure joint working and consistent messaging. For example, trusts in the North West worked together to develop a consistent visiting policy.
The trust's command and control structure worked particularly well both for the trust and in the local system, with representation from the ambulance service, care homes and community teams.
There were examples of good support to care homes, including support with PPE, testing and training. For example, to avoid hospital attendance, one trust provided therapy teams to care homes, supported by fortnightly calls and IPC training and supplies.
One trust supported their local prison with remote outpatient appointments and provision of some PPE, and helped them to develop their response in the event of a COVID-19 pandemic.
Care homes
During August, we carried out a special programme of inspections of infection prevention and control (IPC) in 300 care homes selected as potential examples of where IPC was being done well. We have been encouraged by the findings so far:
- Very few of these services turned out not to be managing well and requiring a fuller inspection.
- Across the 300 inspections, we’ve had more than 90% assurance across all the elements we were looking at.
- Feedback from the initial inspections has identified good practice examples, such as these:
Staff had organised an Eid dinner via [video conference] for a person who had always shared this with their family. Staff decorated the room and played the video link through a large television. The manager told us this made the person feel they were sitting at the table with their family.
Staff bought face coverings to suit people's personality and interests to encourage their use. For example, one person who is very keen on public transport has a mask with buses on it. Another person who loves anything military has been given a camouflage mask.
Staff introduced new indoor activities, such as themed nights. Providers invested in new equipment for the garden to keep people engaged, for example a large outdoor above-ground swimming pool. Resident surveys are completed regularly to monitor people's wellbeing and assess their needs during the pandemic.
We will report fully on the findings of this programme in November.
The following section focuses on the evidence we collected during 59 high-risk inspections of care homes during the first half of August 2020. These were inspections carried out specifically in response to concerns about safety and quality, or to feedback from staff or people using services and their families.
During these inspections we reviewed how well staff and people living in care homes are protected by IPC, looking at assurance overall and across eight key areas.
Despite these being services where we may have had concerns about quality, we were assured or somewhat assured in all areas of good IPC in the majority of services (figure 2). The findings allow us to review the two areas where we had greatest assurance, in safe admission and IPC for visitors, as well as the two areas where we had least assurance, IPC policy and effective use of PPE. This highlights areas of relative strength, as well as the gaps and barriers most commonly missed by services, which providers can use to reflect on and improve their practice.
Where CQC has been assured that people are protected, we will not need to take any further action. However, in cases where we have concerns, we can take a range of regulatory action, including issuing lower-level requirement notices, through to warning notices and, in cases of significant concern, placing conditions on a provider’s registration.
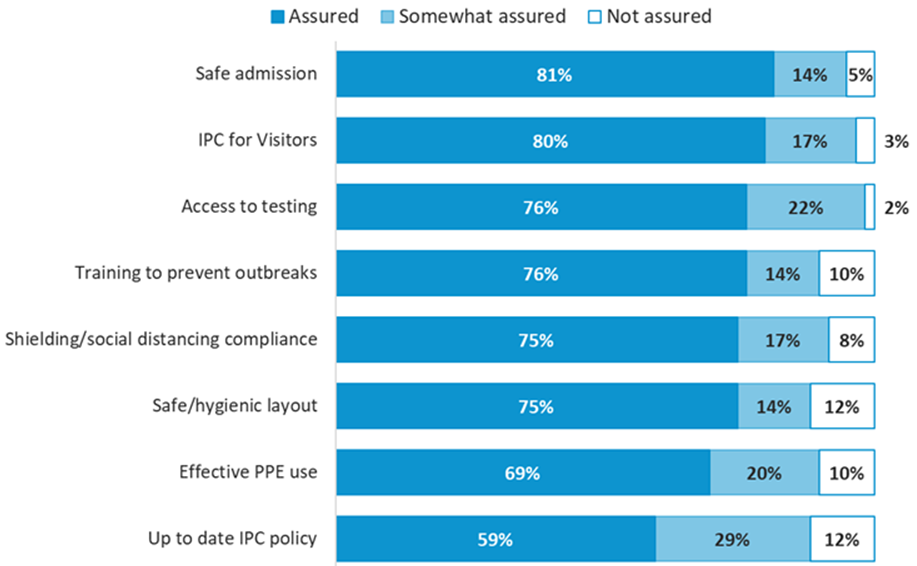
Source: Responses from 59 risk-based care home inspections across all questions.
Safe admission
We were assured in more than four-fifths of care homes in our risk-based inspections that the homes were following the guidance in relation to safe admissions. This included carrying out tests to make sure they knew people’s COVID-19 status. Some care homes would only accept people from hospital with a negative test. Others had procedures in place to safely accommodate people while they awaited test results. This required the person to be cared for in isolation until a negative test was obtained, by allocated staff who always wore appropriate PPE.
Current measures in place are person is escorted to their bedroom – set up a PPE station outside their room – clothes are labelled so they are left for 72 hours. Staff will be in full PPE.
Examples were provided to demonstrate how all new admissions had isolated for 14 days, including those returning from a hospital visit. Care homes carried out routine monitoring throughout the isolation period. Other homes routinely monitored all the people who lived there and had procedures in place should they identify concerns.
A few services had a ‘no new admissions’ policy in place.
There was some evidence to suggest services had considered the Mental Capacity Act, Deprivation of Liberty Safeguards and best interest decisions around COVID-19 and isolation for those who lacked capacity.
IPC for visitors
We were assured in four-fifths of care homes in our risk-based inspections that all types of visitors were prevented from catching and spreading infection.
Care homes’ approaches to visiting should be appropriate for the service and consider and meet the needs of people living in them. Care homes we inspected had different visiting policies, ranging from a few that still had a ‘no visitors’ policy, those that were facilitating window or garden visits, through to a few that were now allowing essential visitors into the home. Inspectors were assured, however, that the different approaches taken by these homes were appropriate for the service and the people living in it, and managed well.
For one person with a learning disability there are special arrangements for a relative to visit, which greatly relieves his anxiety. A special room is set aside for them and PPE is worn at all times.
Where no visitors were allowed into the home, there was usually an exception for people receiving end of life care.
When visitors entered a care home there were often screening procedures in place, such as a questionnaire or declaration and temperature checks. PPE was required and, in most cases, provided if the visitor did not have their own. Handwashing facilities and hand sanitiser were available, and their use prompted by staff. Inspectors saw good signage at the entrance to care homes and reminders throughout the home.
It was most common for visits to be supported in the garden, which could be accessed without entering the care home. If the weather was poor some services had identified indoor spaces, which again could be accessed without entering the main body of the home. Visitors were required to wear face masks and maintain a safe social distance. Contact with staff members was limited.
Some care homes allowed visits only at open windows, by appointment to avoid crowding. Another service allowed relatives to come in their car and see their relative or friend through the open car window. Care homes had written to families to explain their visiting policy and the majority had alternatives to face-to-face visiting. Inspectors described how people living in the care home were supported to contact their relatives and friends by video.
Provider had offered [app] to people using services’ families free of charge during COVID-19…to keep them up to speed with their relative’s care, daily activities and wellbeing. Staff take photos and videos of the person and send them to families, who can respond back. The home also bought two portals to facilitate visual, real-time interaction between people using services and their families.
Visits tended to be by appointment only, restricted to one visitor at a time and staggered to allow cleaning between visits. Inspectors were assured by seeing the policy in action.
IPC policy
We found the lowest level of assurance (59%) against the question, “Is your IPC policy up-to-date and implemented effectively to prevent and control infection?”. Inspectors reviewed each care home’s policy and interviewed staff to understand whether it had been implemented effectively. We found examples of IPC policies that were out-of-date. Some had been updated early on in the COVID-19 pandemic but had not been amended since and so contained out-of-date information. This posed a risk to the staff and people who live in the care home. Others had not been updated since 2019.
Another barrier to effective infection prevention control was limited, or a lack of, contingency planning. One care home had completed a plan, but it only covered the hot weather and did not include preparations for autumn and winter.
We also found examples of care homes that lacked risk assessments for people from Black and minority ethnic groups and others who were at higher risk due to the pandemic, as well as for staff members. Our inspectors also found that risk assessments for these groups had not been actioned.
Effective use of PPE
The second lowest area of assurance in these risk-based inspections (69%) was whether services used personal protective equipment (PPE) effectively to safeguard staff and people using services. In care homes where PPE was not worn at all or not worn correctly, IPC was compromised. This was seen in different areas of the homes, such as during break times, while handling or serving food, and when in close proximity with the people they provided care for. There were instances where it was only one member of staff who was not using PPE correctly, through to no consistency with its use among different staff members.
In one service we found staff were not changing masks due to limited supplies. They said that PPE supplies were restricted and they had to request supplies throughout the shift because they were locked away, with only the manager and lead domestic having access.
PPE should be stored safely in a clean, dry area to prevent contamination1. We observed care homes that lacked a specific area for donning and doffing PPE, which could lead to contamination of other surfaces, and PPE that was stored uncovered.
There are no specific donning and doffing stations. Staff use the staff toilet to do this, or don and doff in corridors where the aprons and gloves are kept, and not always covered to prevent cross infection. Observed aprons hanging over towel rails – not covered. Saw much of the PPE not covered.
Another barrier to effective infection prevention control was PPE that was not disposed of correctly as healthcare waste. We also found that appropriate bags for the disposal of used PPE were not always available. Inspectors saw PPE in regular waste bins that had not been sealed and bagged separately.
GP surgeries
This section highlights some of the infection prevention and control (IPC) measures taken by GP surgeries in response to the COVID-19 pandemic. The findings are drawn from conversations with 43 GP surgeries to understand what they have done, as well as good practice they want to share and challenges they have faced.
PPE and cleaning procedures
Respondents were generally positive about the use of personal protective equipment (PPE), telling us that staff and patients or visitors were wearing appropriate PPE and were practising regular handwashing. Practices reported that people complied with wearing face coverings and clinical staff donned gloves, visors and full scrubs where appropriate. These were appropriately changed between patients.
They told us that staff training and access to PPE for clinicians had improved. For example, disposable aprons and gloves were stored around the service, and ‘grab-bags’ of PPE were readily available for home visits.
While PPE supplies were being regularly audited and availability had generally improved, some services had experienced difficulties in obtaining adequate stock in a timely manner, especially during the early stages of the pandemic.
GPs also told us that hygiene and cleanliness had improved as a result of the pandemic. Cleaning schedules were widely enhanced, and staff were proactive, allowing themselves enough time between patients to disinfect workstations and rooms.
Social distancing and minimising patient contact
GP practices were able to reduce the number of face-to-face consultations, including home-visits, through the use of remote triaging. Video and phone consultations, and ordering prescriptions direct to pharmacies, played an important role in reducing footfall in services, meaning that only patients with the greatest need were attending appointments in person.
A number of services told us that they were taking patients’ temperatures on arrival and screening for COVID-19 symptoms. They also introduced ‘hot zones’, or designated areas of the service to see patients with suspected symptoms. They said this has helped to contain potential infection, identify where and when full PPE should be worn, and target deep cleaning.
Services commonly adopted a ‘locked door policy’ to minimise the number of people in a service at any one time. The use of intercom, chaperoning and one-way systems further facilitated social distancing and limited the time spent in the building. Perspex screens were often fitted in reception areas, and waiting rooms were reconfigured to allow for space between people. One practice converted their car park into a temporary waiting area and another operated a system where visitors could be collected from their cars.
The GP practices we spoke to said they have implemented some innovative ways to reduce the risk of infection for people who use services. For example, we heard that some services have staggered clinic times, seeing people who are most vulnerable early in the morning, and holding ‘one-stop’ clinics for people with more complex/co-morbid conditions such as diabetes.
We heard of other cases where services have worked in new ways to best respond to people’s needs during the pandemic. For example, some services have introduced welfare calls with certain patients to offer ongoing remote support. Other GP practices have worked with other agencies to best respond to local needs.
The homeless community were particularly vulnerable to infection and without anywhere to quarantine. Initially we closed the car park and bought tents in for symptomatic patients until we were able to find some accommodation. But then when national funding arrived, we worked with the council to set up ‘care and protect’ hotels; one of these is always a symptomatic patient site, where patients can be triaged, tested and quarantined. We’re still supporting all these sites with daily GP and nurse rounds.
These changes in the way GP practices are working have not come without cost. For example, we were told that some staff and patients have felt increased levels of stress and frustration with remote care.
There were also some concerns that some non-urgent patients who require procedures like routine screening and immunisation are not being seen in a timely manner because they are worried about contracting COVID-19 during a visit to the surgery, or because they think their GP could lack capacity to see them. This may be having implications on patients’ health.
Guidance/communication around COVID-19
There have been mixed messages around the clarity and effectiveness of communication around national IPC guidance. Respondents raised concerns that messages, particularly in the early stages of the pandemic, were inconsistent and confusing.
However, they also told us that communication around IPC practice within services and with local stakeholders, such as clinical commissioning groups and local authorities, has been good, with many examples of daily meetings.
Working closely with the other GP practice and services located within the health centre ensures a consistent message regarding infection prevention and is sent to all patients entering the centre.
Communication with patients was viewed as positive, with people being kept informed via text messages, social media alerts and websites. Many practices said they had made a great effort to regularly contact patients that were hard to reach and those with chronic and mental health conditions, to ensure they were fully informed of the implications of the COVID-19 pandemic on their ongoing care.
IPC audits
The majority of respondents told us that they had carried out IPC audits before or as a result of the pandemic, making changes and improvements to mitigate the risks identified. This often meant that cleaning schedules were enhanced, non-wipeable furniture was replaced in practices, and IPC record keeping improved. Some services told us that they are now carrying out more regular IPC audits to monitor and identify issues, such as stock of PPE, to ensure they are continuing to maintain as safe an environment as possible.
Read more...
Download the report
You can download a version of this report if you want to print or share it with your team.
Related news
You can read our news story about this issue of the report:
Keeping people safe and supported through the pandemic.
Previous issue
You can read the issue of the report that we published in July. This issue looked at how providers were working together, how we respond to feedback about care, the financial viability of social care and the impact on the use of the Deprivation of Liberty Safeguards.