Effective infection prevention and control (IPC) is essential to protect people from acquiring COVID-19. Providers need to make sure they are taking action to minimise the risk of cross-infection.
During August 2020, we carried out a special programme of IPC inspections in 301 care homes selected as potential examples of where IPC was being done well. We have also reviewed IPC in 139 ‘risked-based’ inspections between 1 August and 4 September, which were carried out in response to concerns about safety and quality. During these inspections, we reviewed how well staff and people living in care homes were protected by IPC measures, looking at assurance overall and across eight questions.
Across the 440 inspections, we found a high level of assurance in the eight questions (figure 1). At 288 of the 440 services visited (65%), inspectors were assured in all eight of the IPC questions.
Effective use of personal protective equipment (PPE) and having up-to-date policies in place were the two areas with the most gaps in assurance.
Wherever inspectors encountered poor practice, they escalated this at the time with the manager of the service and signposted to the available guidance. In a few cases an inspector returned to complete a comprehensive inspection or pursued regulatory action.
As would be expected, the care homes selected as potential good practice examples generally demonstrated higher levels of assurance across the eight questions than those where we carried out risk-based inspections.
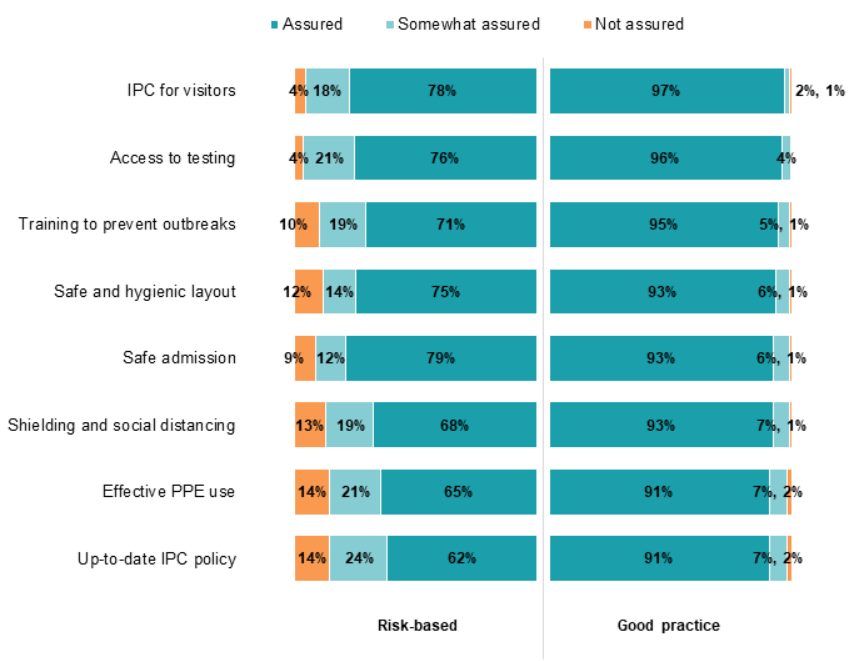
Note: 'Good practice' care homes were those selected for potential good practice; 'Risk-based' care homes were inspected due to concerns over quality and safety.
Access to visitors
IPC for visitors obtained the highest level of overall assurance (91%), with care homes working hard to comply with visitor guidance. Restrictions have come at a price, however, with many people using services feeling the impact of not seeing their families and carers in the way they are used to.
"Relatives have been upset and have found it hard not visiting. Informing people and relatives has been very important to develop their understanding around why rules are in place. [Provider] uses two main means of communication – writing to them every week with updates about what’s going on, and a question and answer document to support staff to answer questions."
Good services had effective systems in place to ensure visiting could go ahead safely. They took a person-centred approach to individual situations to ensure people’s needs were met. Garden visits were well supported and homes looked for methods to keep people in touch with loved ones and the community that did not rely on people meeting face-to-face.
There were some challenges to ensuring social distancing during visits and some signage and screening procedures could have been improved.
Robust systems for screening and PPE for people entering the service were seen to be successful in preventing the spread of infection.
There are considerations for all providers going forward on balancing visiting restrictions based on current, local advice, against the rights, health and wellbeing of people who use the service and the risk of harm from isolation.
Shielding and social distancing
Most services had suitable plans in place to care for people who are symptomatic or COVID-19 positive and protect others living in the care home in the event of an outbreak. Social distancing was promoted and maintained wherever possible.
Good services took a person-centred, risk-assessed approach, and took simple practical steps to support people where social distancing was a challenge (for example, when delivering personal care or supporting people living with dementia).
To mitigate the impact of isolation good services provided meaningful activities and ensured people were included in the conversation about their isolation so they better understood it.
"A person recently admitted to the home had to spend 14 days in isolation. Staff found out he was a keen cyclist. They have purchased a pedal exerciser and he is currently cycling from Bradford to Portsmouth. Staff have been talking to people about the challenge he set himself and this has helped him integrate into the service while in isolation."
Good practice included supporting people to access the community safely as lockdown restrictions eased.
Where inspectors found gaps in assurance this most commonly related to services that had not considered social distancing in the layout of their services and where staff did not maintain this in their interactions with each other.
Safe admissions
Good services carried out effective admission assessments despite the challenges, considered mental capacity and took action to reduce the impact of isolation.
Services routinely tested and isolated new admissions to help prevent the spread of infection.
"The service undertook non-face-to-face assessments using video calls, talking to family and the hospital/social worker to get as much information as they could. The care home insisted the person had a negative swab as close to admission as possible with evidence of this."
Gaps and challenges were reported where 14-day isolation on admission had not taken place.
While some services admitted new people after appropriate assessment, others made blanket decisions to refuse admissions. This had potential consequences, both in terms of financial viability and local capacity.
Effective use of PPE
Whether services used personal protective equipment (PPE) was the second lowest area of assurance.
Despite challenges at the beginning of the pandemic, the supply of PPE was seen to be working. Generally, inspectors were assured that staff understood the PPE guidelines and that safe procedures had been implemented.
Good examples of IPC using PPE began from the moment that staff arrived at work, where they would enter the separate donning/doffing area and remove the clothes that they travelled to work in to prevent contamination.
Staff wearing PPE could be difficult for people who use services. Good services engaged with people to provide reassurance, support and understanding. Risk assessments into the use of PPE were carried out as appropriate.
Good services promoted a culture of responsibility and engaged staff in the use of PPE, encouraged by ‘champions’.
"Two or three IPC leads undertook further training to become part of the 'IPC Army'. They were given extra time to undertake additional IPC responsibilities such as PPE competency checks and assisting with more frequent audits."
Where inspectors found gaps in assurance this related to a lack of compliance with guidance on donning and doffing of PPE, mask wearing and handwashing. Safe disposal of PPE was also an area of some concern.
Testing for staff and people who use the service
Good services had an enthusiastic, well-managed approach to testing and demonstrated going the extra mile to achieve this. Although they encouraged people who receive care to take tests, they respected their rights to refuse testing, and would risk assess them individually and consider capacity and best interest decisions.
Many providers saw routine and regular testing as vital, especially with the risk of asymptomatic spread.
"Started regular testing as soon as it was available. Very enthusiastic about this; we have a spreadsheet tracker of everyone, weekly for staff and monthly for people using services. Took the view that if cases could be asymptomatic it was crucial to do regular testing. This approach appears to have been a key factor in reducing spread of the virus."
Where inspectors found gaps in assurance this related to a small number of services that had made no effort to implement testing or they did not properly understand the expectations.
Although inspectors were assured that care homes were taking part in testing schemes and doing everything they could to apply guidance, this does not reflect the delays reported by providers in obtaining testing kits during August. This was deemed to be outside of the homes’ control by inspectors but impacted on their ability to deliver testing at the required frequency.
Layout of space and hygiene practices
Though it has always been important for care homes to be clean and hygienic, the nature of the pandemic has put these practices under the spotlight.
Services were generally clean and hygienic. Some services had removed excess furniture, decluttered and made changes to flooring and furniture covers to facilitate easier cleaning.
Some services did not have good access to spare single-occupancy rooms or en-suite facilities. In these cases, managers had to make decisions on how to balance the pre-existing needs of people while also planning for possible outbreaks.
Services recognised the considerable impact of moving people from the room that they are used to, to another room for cohorting, isolation or shielding – particularly for those with dementia.
"Manager advised that if another resident tests positive they will try to move them to the empty bedrooms rooms downstairs. He said that not all of the residents there would agree to their room being moved and if this was attempted it could be very distressing for them."
Staffing and staff training
Inspectors saw examples of very good staff practice across the services they visited. Staff demonstrated resilience to work under such uncertain circumstances and commitment to care for the people using services and their colleagues.
Most staff had received training and possessed good knowledge of infection prevention and control practice, and generally felt well supported.
"All staff can complete a ‘health reflection form' to gauge how staff feel about the emotional and physical impact so far. Staff who would not speak out found a voice in the support mechanisms."
Staff were often cohorted or assigned to areas to minimise movement and cross-infection. Reflecting the findings in a survey carried out between May and June 2020, a lot of services were not using any agency staff to limit the risk of cross-infection from other services.
IPC policy and contingency planning
IPC policy and contingency planning was one of the most variable areas, and where we saw the least assurance.
There were services that had reviewed and updated their policies and these were communicated well with staff. In contrast, there were IPC policies that had not been updated since the start of the pandemic and contained no reference or out-of-date guidance on COVID-19, which had the potential to be dangerous.
Some services have learned from the first wave of the pandemic and could give examples and reflect on things that did not go well and what actions were taken to change that. Services also asked for feedback from the people who live at the care home and their relatives to understand how they could improve.
"The prevention and protection plan was very detailed and shared among all the staff about what plans are in place for how to manage a possible second wave. It includes an outbreak checklist, role specific responsibilities and top tips, a symptoms checker, a standard cleaning process, housekeeping and catering teams top tips, hand hygiene guidance, PPE guidance for cohorting and zones, and cohorting guidance in the care home."
Read more...
Download the report
You can download a version of this report if you want to print or share it with your team.
Full reports
You can read our full report on infection prevention and control in care homes or the results of our survey of COVID-19 inpatients:
- How care homes managed infection prevention and control during the coronavirus pandemic 2020
- Inpatient experience during the coronavirus (COVID-19) pandemic
Related news
You can also read our news stories about the publication of these reports:
- CQC publishes Infection Prevention and Control inspections report
- CQC reports on the findings of its coronavirus (COVID-19) inpatient experience survey
Previous issue
You can read the issue of the report that we published in September. This issue looked at how infection prevention and control and provider collaboration reviews.