Regulations for service providers and managers
Notifiable safety incidents
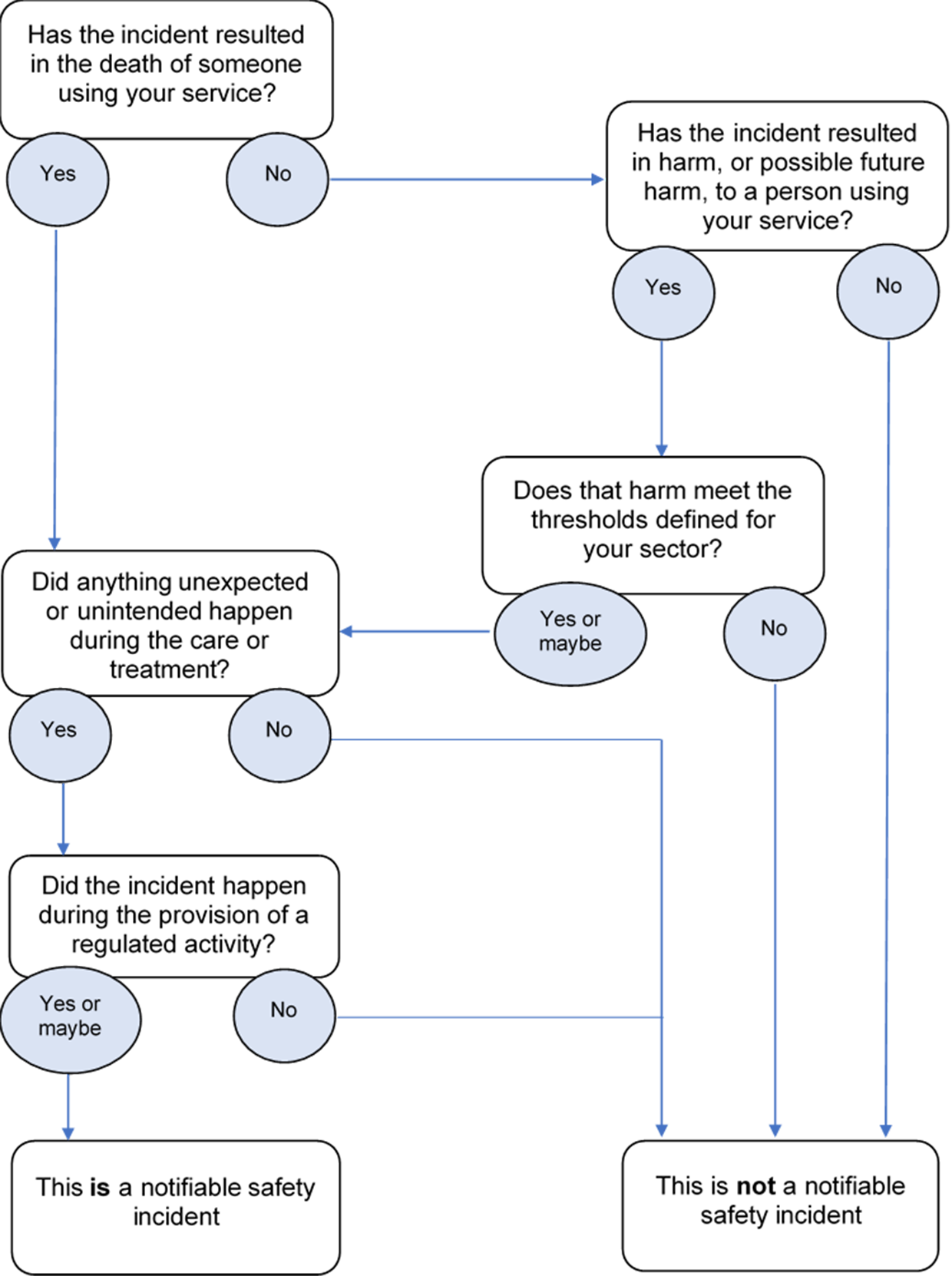
The changes clarify how you should apply the term “unexpected or unintended” to decide if something qualifies as a notifiable safety incident or not.
See updated pages:
‘Notifiable safety incident’ is a specific term defined in the duty of candour regulation. It should not be confused with other types of safety incidents or notifications.
A notifiable safety incident must meet all 3 of the following criteria:
- It must have been unintended or unexpected.
- It must have occurred during the provision of an activity we regulate.
- In the reasonable opinion of a healthcare professional, already has, or might, result in death, or severe or moderate harm to the person receiving care. This element varies slightly depending on the type of provider.
If any of these three criteria are not met, it is not a notifiable safety incident (but remember that the overarching duty of candour, to be open and transparent, always applies).
You should interpret "unexpected or unintended " in relation to an incident which arises in the course of the regulated activity, not to the outcome of the incident. By "regulated activity" we mean the care or treatment provided. By "outcome" we mean the harm that occurred or could have occurred. So, if the treatment or care provided went as intended, and as expected, an incident may not qualify as a Notifiable Safety Incident, even if harm occurred.
This does not mean that known complications or side effects of treatment are always disqualified from being Notifiable Safety Incidents. In every case, the healthcare professionals involved must use their judgement to assess whether anything occurred during the provision of the care or treatment that was unexpected or unintended.
The definitions of harm vary slightly between health service bodies and all other providers. This is because when the regulation was written, harm thresholds were aligned with existing notification systems to reduce the burden on providers.
It is possible for an incident to trigger the harm threshold for NHS trusts, but not for other service types, or vice versa.
It is helpful to remember that the statutory duty relates to the provision of regulated activities, and so you should follow the notifiable safety incident definition relating to the type of organisation or provider you are working within.
Health service body
Section 9 of the National Health Service Act 2006 defines a ‘health service body’. For the purposes of the duty of candour, a health service body means either an:
- NHS trust
- NHS Foundation trust.
Paragraph 8 of Regulation 20 defines the harm thresholds for Health Service Bodies:
In the reasonable opinion of a healthcare professional, the incident could result in or appears to have:
- resulted in the death of the person - directly due to the incident, rather than the natural course of the person's illness or underlying condition
- led to the person experiencing severe harm, moderate harm or prolonged psychological harm.
These definitions of harm are linked to the National Reporting and Learning System (NRLS) definitions.
All other services we regulate
Paragraph 9 of Regulation 20 defines the notifiable safety incident harm thresholds for all other services we regulate:
In the reasonable opinion of a healthcare professional, the incident appears to have resulted in, or requires treatment to prevent:
- the death of the person - directly due to the incident, rather than the natural course of the person's illness or underlying condition
- the person experiencing a sensory, motor or intellectual impairment that has lasted, or is likely to last, for a continuous period of at least 28 days
- changes to the structure of the person's body
- the person experiencing prolonged pain or prolonged psychological harm, or
- a shorter life expectancy for the person using the service.
These definitions of harm are aligned to CQC’s notification system for reporting deaths and serious injuries.
Definitions of harm
These definitions are common to all types of service.
Moderate harm
Harm that requires a moderate increase in treatment and significant, but not permanent, harm.
Severe harm
A permanent lessening of bodily, sensory, motor, physiologic or intellectual functions, including removal of the wrong limb or organ or brain damage, that is related directly to the incident and not related to the natural course of the service user's illness or underlying condition.
Moderate increase in treatment
An unplanned return to surgery, an unplanned re-admission, a prolonged episode of care, extra time in hospital or as an outpatient, cancelling of treatment, or transfer to another treatment area (such as intensive care)
Prolonged pain
Pain which a service user has experienced, or is likely to experience, for a continuous period of at least 28 days.
Prolonged psychological harm
Psychological harm which a service user has experienced, or is likely to experience, for a continuous period of at least 28 days.
Identifying a notifiable safety incident
The presence or absence of fault on the part of a provider has no impact on whether or not something is defined as a notifiable safety incident. Saying sorry is not admitting fault.
Even if something does not qualify as a notifiable safety incident, there is always an overarching duty of candour to be open and transparent with people using services.
Flow chart: updated 30 June 2022
Patient gave consent
Something can qualify as a notifiable safety incident even if the patient gave consent for a procedure to be carried out. It all depends on the level of harm and whether something unexpected or unintended happened during the care or treatment, regardless of whether consent was given.
Notifiable safety incident occurred in a different provider
If you discover a notifiable safety incident that occurred in a different provider, you should inform the previous provider.
You must also be open and transparent with the person receiving care about whatever you have discovered. But you do not need to carry out the specific procedures relating to notifiable safety incidents.
The provider where the incident happened must carry out the notifiable safety incidents procedures.
Multiple providers contributed to the harm
If multiple providers contributed to the harm, they should liaise and work together in the investigation that follows as they would for any other incident. Each provider still has its own responsibilities under the duty of candour. They must assure themselves that they have met them.
Incidents that occurred before the duty of candour came into force
There is no legal requirement to carry out the specific requirements laid out in Regulation 20 for something that happened before the regulation existed. However, we would still expect you to carry out the general duty of candour – to apologise and to be open and transparent with people about whatever has been discovered.
Retrospective reviews and patient recalls
If the notifiable safety incident was not realised at the time but was discovered through a retrospective case review, or as part of a large scale patient recall, the duty still applies.
Incidents where there are no staff actively caring for the person
For example, this might be where a person has an unwitnessed fall in a care home.
The care being delivered is described by the regulated activity. In this example that is ‘accommodation for people who require nursing or personal care’. The person fell during the delivery of the accommodation part of the regulated activity. So provided the harm thresholds are met, this could qualify as a notifiable safety incident.
Return to theatre following surgery or a transfer to another treatment area
The term ‘moderate increase in treatment’ does include situations such as a transfer or an unplanned return to surgery. But ‘moderate increase in treatment’ is only one part of the overall definition of ‘moderate harm’. And it is the description of ‘moderate harm’ that helps define if something is a notifiable safety incident. To meet the ‘moderate harm’ threshold the harm must require a moderate increase in treatment and there must be significant, but not permanent, harm.
So a transfer or unplanned return to theatre does not automatically qualify as a notifiable safety incident.
Near misses
The intention of the term “could result in harm” in the harm definitions is not to bring near misses into scope as notifiable safety incidents. It is designed to reflect harm that is not apparent at the time of the incident but that may appear later.
See some worked examples of notifiable safety incidents.