This is the 2019/20 edition of State of Care
In last year’s State of Care report, we spoke about how high-quality care was not always as easily accessible to people with some protected equality characteristics. Many of the same quality and accessibility issues continued in 2019 and into 2020. In the 2019 adult inpatient survey, which asked more than 75,000 people about their experiences at acute NHS trusts, people with dementia, people with mental and behavioural conditions, and younger adults in the 16-35 age group all consistently reported poorer experiences of care than others. Separately, data from NHS Digital showed that people in the most deprived areas of England were almost twice as likely to visit A&E as those in the least deprived areas in 2019/20.
Navigating the complex health and social care system, and the services within them, is not always easy. This is partly because different services work individually, rather than in partnership. This affects people with some protected equality characteristics more negatively than others, and puts those whose preferred language is not English (including British Sign Language users) at a disadvantage from the beginning, as information about services and how to navigate care pathways is not always accessible to them and interpretation services are not always available.
We have heard from inspectors and external stakeholders of considerable variation between different areas and services in how well they consider the needs of people from different groups – particularly people from Black and minority ethnic (BME) groups, people from religious groups and disabled people. We also heard that the needs of people experiencing homelessness, prisoners, and people who experience distress that leads to behaviour that services find difficult, may not always be adequately planned for.
As well as for people using services, inequality affects staff working in the health and social care system. For people who work in the NHS, the Workforce Race Equality Standard (WRES) and the Workforce Disability Standard (WDES) give us information about how people from BME backgrounds and disabled people fare in their workplaces, compared with their white and non-disabled colleagues.
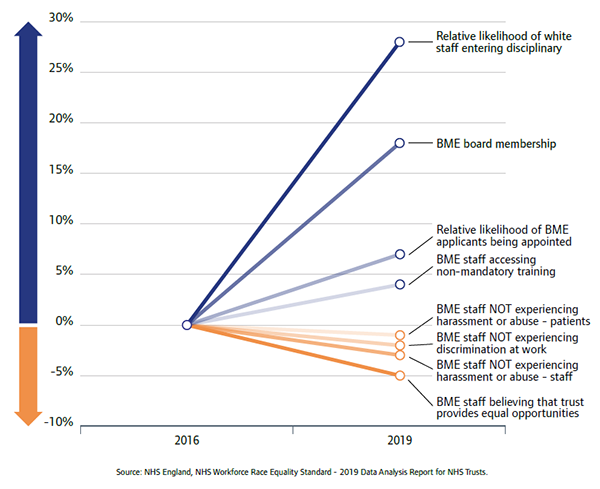
Nationally, there has been a variable amount of change in the key WRES indicators over the four years of annual WRES reports. Figure 6 shows that there has been marked improvement in some areas, such as BME board membership and equal treatment in whether staff from BME groups and white groups enter disciplinary proceedings. For other indicators, such as those concerned with harassment and discrimination at work, there has been a slight decline for staff from BME groups.
WDES is a newer standard, and this is the first year we have reported on it here. The NHS England 2019 annual report on WDES showed that disabled people felt less valued, were less likely to be appointed during recruitment, had lower engagement scores, and felt they were less likely to be considered for promotion than non-disabled people. Disabled people were found to be more likely to be subject to bullying, abuse and harassment, pressured to work when unwell, or subject to formal capability processes than their non-disabled colleagues. Disabled people are under-represented on boards.
We are committed as a regulator to consider workforce equality in our assessment of whether trusts are well-led, so we were pleased to see that NHS England and NHS Improvement have also emphasised their ambitions in this area. In July, they published an update to their people plan, which sets out their plans to improve inclusive employment practices and develop better support for the wide variety of people who work in the NHS.
Next page
Part 2: The impact of the coronavirus pandemic
Previous page
This is the 2019/20 edition of State of Care.
Go to the latest State of Care.
Contents
Quality of care before the pandemic
- Quality overall before the pandemic
- Care that is harder to plan for was of poorer quality
- Care services needed to do more to join up
- Adult social care remained very fragile
- Some of the poorest quality services were struggling to make any improvement
- There were significant gaps in access to good quality care
- Deprivation of Liberty Safeguards
- Inequalities in care persisted
The impact of the coronavirus pandemic
- The impact on people
- The impact on health and social care staff
- Infection prevention and control
- The unequal impact of COVID-19
- The impact of COVID-19 on DoLS
- Innovation and the speed of change
Collaboration between providers
- How did care providers collaborate to keep people safe?
- System-wide governance and leadership
- Ensuring sufficient health and care skills where they were needed
- The impact of digital solutions and technology
