This is the 2019/20 edition of State of Care
The impact of COVID-19 on people in terms of delays to elective and diagnostic care is enormous. In real terms, this means people who have not yet had the life-changing operations they need, and people whose cancer remains undiagnosed or untreated.
The increased waiting lists and backlog of urgent and elective care need to be addressed. Services need to assess and prioritise patients so that they are treated according to clinical need and that people waiting for long periods for treatment are kept safe. There must be learning to make sure these services are protected in any further resurgence of COVID-19.
The decline in the numbers of people attending emergency departments at the start of the pandemic made it more possible for hospitals to manage patient flow in a safe and effective way. It is worth noting that, while performance against the 95% four-hour target has not been met since July 2015 (falling to its worst level in December 2019), the reduction in attendances enabled emergency departments to get back close to achieving the 95% target in May, although performance has since fallen as attendances have begun to rise (figure 15).
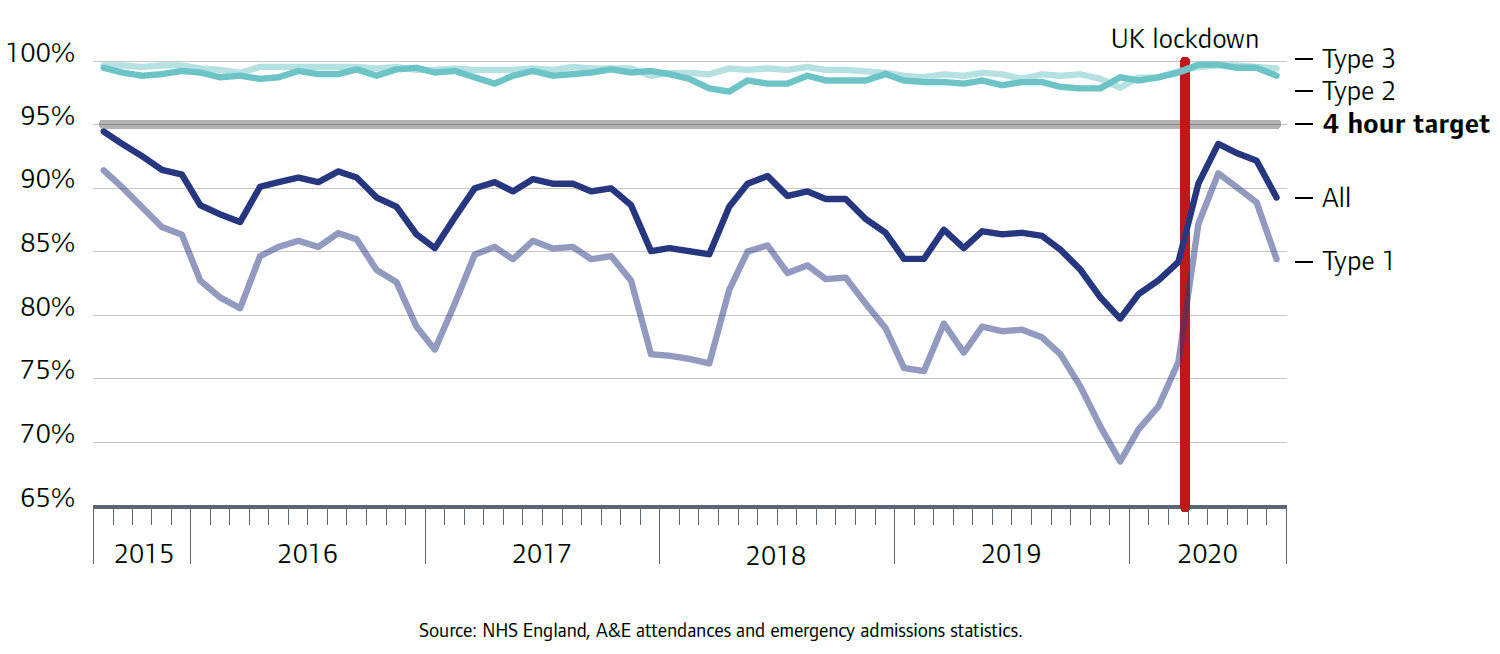
Source: NHS England, A&E attendances and emergency admissions statistics
Since May the numbers of people attending urgent and emergency care have been increasing. There are concerns that this heightened demand and continued workforce pressures could lead to a return to the overcrowding in emergency departments and corridor care that was seen last winter. Balancing this increasing demand alongside continued COVID-19 care brings significant challenges – particularly as we head into winter, with the additional risk that subsequent spikes of the virus may coincide with seasonal flu.
We have worked with a group of frontline clinicians from good and outstanding emergency departments across the country to better understand what lessons can be learned from the initial impact of COVID-19 and what good practice can be usefully shared to support long-term service improvements. This resource includes examples of closer working between departments and greater collaboration between hospitals, primary care and community services that can help increase capacity, ensure robust infection control, allow effective social distancing, and support patients to access the service most appropriate to their needs.
Effective infection control will remain essential to protect people from acquiring COVID-19. Providers need to make sure they are taking action to minimise the risk of cross infection. This includes – like for all health and care services – maintaining the highest standards of infection control in all areas, as well as mitigating the challenges caused by social distancing rules, such as reduced capacity in waiting rooms and reception areas.
This applies equally to controlling the spread of COVID-19 between different services. It is essential that information about patients’ COVID status is shared appropriately and in a timely way, so that all health and care professionals are able to take steps to protect themselves and everyone else in their care.
Going forward, hospitals and other healthcare services need to finely balance the capacity to provide COVID and non-COVID care, and make sure that people have the confidence to come forward for the care and treatment they need.
Working closely with other local care providers will be crucial. Those working in acute healthcare services need to take this step and move beyond their natural boundaries. Forming closer partnerships and working as one integrated system has never been more important than now.
Next page
Previous page
This is the 2019/20 edition of State of Care.
Go to the latest State of Care.
Contents
Quality of care before the pandemic
- Quality overall before the pandemic
- Care that is harder to plan for was of poorer quality
- Care services needed to do more to join up
- Adult social care remained very fragile
- Some of the poorest quality services were struggling to make any improvement
- There were significant gaps in access to good quality care
- Deprivation of Liberty Safeguards
- Inequalities in care persisted
The impact of the coronavirus pandemic
- The impact on people
- The impact on health and social care staff
- Infection prevention and control
- The unequal impact of COVID-19
- The impact of COVID-19 on DoLS
- Innovation and the speed of change
Collaboration between providers
- How did care providers collaborate to keep people safe?
- System-wide governance and leadership
- Ensuring sufficient health and care skills where they were needed
- The impact of digital solutions and technology
